Introduction. Endocrine disorders and impaired gonadal function are the most frequent sequelae after transplantation.
Methods. Male patients <18 years transplanted in the period 1992-2021 in the Pediatric Transplant Unit in Monza, surviving more than 2 years after HSCT, who either experienced spontaneous puberty (Tanner stage ≥2, testicular volume (TV) ≥4 mL or serum testosterone ≥0.2 ng/mL) or received pharmacological pubertal induction were included in this study.
Longitudinal endocrine evaluations were performed every 6-12-months, including Tanner stage and TV assessment and LH, FSH, total testosterone, among laboratory data.
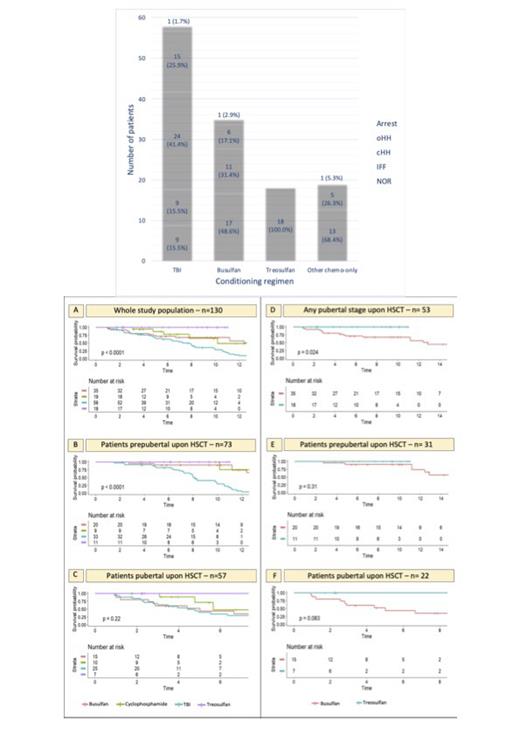
Results. Of 130 patients (median age 9 years at HSCT, 21 years at last follow-up) fulfilling inclusion criteria, 65% were transplanted for acute leukemia, 9% for other malignancies and 26% for non malignant diseases after a TBI (45%), busulfan (27%), 14% treosulfan-based or 15% a different chemo-only conditioning. Upon HSCT 56% were prepubertal (PreP) and 44% where either peri- or postpubertal (PostP). The pubertal status upon the last endocrine evaluation was consistent with Tanner stage 3, 4 and 5 in 15%, 23% and 62% of the patients, respectively.
Overall, 44% had spontaneously progressed into puberty and had a normal gonadal profile (NOR) and 56% had experienced either pubertal arrest (1%), isolated increase of FSH (IIF 19%), compensated hypergonadotropic hypogonadism (cHH, 23%) or overt hypergonadotropic hypogonadism (oHH, 13%).
Gonadal outcome was not affected by pubertal status upon HSCT (p 0.298), even though, out of 81 patients who had achieved Tanner stage 5, TV was statistically greater in the PostP (12.2±5.1 ml) than in the PreP cohort (10.3±4.1 ml, p 0.049), whereas there were no significant differences in the last testosterone level recorded in the two cohorts, as well as in the hypogonadal versus the event-free patients (p 0.53), with events defined as any gonadal issue (IIF, cHH, oHH). TV was significantly lower in patients who developed any endocrine disfunction versus those who didn't.
LH and testosterone levels showed a specular trend between 20 and 30 years, when a progressive decrease in sexual steroids was associated with a compensatory increase of the luteinizing hormone. Overall, adult LH (p 0.728) as well as FSH levels (p 0.318) were superimposable in the PreP and PostP cohorts.
In terms of the impact of the conditioning regimen on gonadal outcomes, a certain degree of gonadal dysfunction (ranging from isolated increase of FSH to hypogonadism or pubertal arrest) was recorded in 37% of the patients overall, and in 85% of the patients after TBI, 51% after busulfan and 32% after cyclophoshamide/fludarabine, whereas no abnormal findings were found among the 18 patients exposed to treosulfan.
The likelihood of a gonadal event-free course was lowest for the TBI and busulfan cohorts, both overall (p<0.0001) and for PreP patients (p<0.0001), whereas it was 100% among the 18 patients conditioned with treosulfan-based schedules. A remarkably greater gonadotoxicity was detected in the busulfan compared with the treosulfan cohort (p 0.024), with a similar trend in the PreP and PostP subcohorts. Busulfan/cyclophosphamide-based conditioning regimens were associated with statistically larger median TV (p <0.001), higher testosterone levels (p 0.008) and lower LH/FSH levels (p <0.001) than those exposed to TBI.
Conditioning regimen (p 0.047) and pubertal status upon HSCT (p <0.0001) were the only variables significantly associated with testicular outcomes in the Cox model, with exposure to TBI being associated with a 2-fold increase in the risk of gonadal failure compared to busulfan (OR 1.93, CI 1.08-3.70), whereas being pre-pubertal upon HSCT was protective, as it was associated with a halved risk of developing any degree of testicular damage (OR 0.50, CI 0.26-0.70).
Conclusions. We demonstrated a i. halved risk of developing post-HSCT hypogonadism in prepubertal patients at HSCT, despite overall smaller final testicular volume; ii. downwards trend in testosterone levels after the achievement of full spontaneous puberty compensated by an inverse upwards trend in LH levels; iii gonadal-sparing profile of treosulfan compared to busulfan-based regimens, with a statistically lower occurrence of hypogonadism and a trend towards larger testicular volume, higher testosterone levels and lower gonadotropins.
Disclosures
Biondi:Novartis: Speakers Bureau; Galapagos: Membership on an entity's Board of Directors or advisory committees; Colmmune: Membership on an entity's Board of Directors or advisory committees, Research Funding; BMS: Membership on an entity's Board of Directors or advisory committees; Agmen: Speakers Bureau. Balduzzi:Novartis, Amgen, Medac, Neovii: Speakers Bureau.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal